A US-based healthcare management company provides coordination of healthcare benefit services, including insurance validation, improper payment identification, revenue recovery, claims processing, waste reduction and fraud. In addition to standard healthcare plans, the company supports processing for state and federal government agencies.
THE CHALLENGE
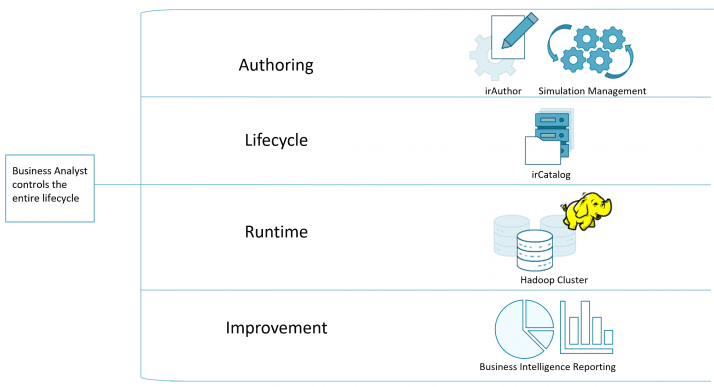
Decision makers sought to improve onboarding time of clients, accelerate improvements and keep control close to the business analysts that know healthcare. Empowering business analysts directly addressed key friction points in the lifecycle of their existing solution.
The company also wanted more frequent simulation of decisions to improve its models and chase down new business opportunities that were previously impractical due to cost.
Driving down the cost of change was not enough. The company selected Hadoop as its alternative to the mainframe. That decision created a new problem—how to run logic at scale.
Finally, with change and performance issues aside, the business required traceability and reporting. The solution had to deliver integration for business intelligence to drive down time-consuming analysis and reporting back to clients.
SOLUTION
In a proof-of-concept, InRule® demonstrated capability to import data, deliver logic in a manner that was easy for the business to understand and run batch processes at scale against Hadoop. This step reduced a lot of integration risk. After that, project stakeholders took part in a business workshop focused on the key problems they wanted to solve. The workshop established the tempo for the project, levels of participation and a playback schedule for rapid designs and deliverables.
As the project unfolded, InRule supported team building activities, best practices and technical training. In the early weeks of the project, business analysts wrote rules everyday growing the shape and complexity of the decisions they needed. At the same time, integration tasks delivered benchmark performance and improvements. In the final stages, InRule delivered specific customizations to the business analysts for batch processing control of scenarios.
The customer used third-party reporting tools for business intelligence without any changes to the InRule solution.
RESULTS
The company now processes over 1 billion claims against Hadoop data in daily batch runs – up from under 100 million with the previous solution. It processes healthcare claims for several states, recovering $6 million per quarter in problem and fraudulent claims.
The project director stated, “The InRule decision platform has given us the ability to scale in ways we never thought we could before, and its support team has been by our side every step of the way. There have been multiple twists and turns throughout the project, but the InRule ROAD and Support teams have been extraordinary in ensuring our project’s success.”
The healthcare company plans to expand its solution to serve more states and payors across the U.S. This growth will push the number of claims processed far into the billions.
“The InRule decision platform has given us the ability to scale in ways we never thought we could before…”
US-Based Healthcare Management Company Project Director


