A U.S.-based healthcare company provides integrated pharmacy benefit management services to health plans, self-insured employers, and government agencies. The company’s services include network pharmacy claims processing, home delivery pharmacy services, drug-utilization review, formulary management, and medical and drug data analysis services.
THE CHALLENGE
The healthcare company relied on a homegrown application integrated with Microsoft Dynamics® CRM to manage its network of doctors, drugs, referrals, billing and payments, and pharmacies.
This application helped direct patients to the company and determined which providers and pricing were available to them. Once a patient saw the doctor, the patient was billed accordingly; if the patient was prescribed a drug, the application determined the appropriate drug based on provider contract and its cost. The healthcare company also sent home health agency employees to administer the drug(s), and the application determined the cost to the patient and the price paid to the agency.
The healthcare company relied on this application to run its business, however, as the business and network expanded, the application became more challenging to maintain. The business rules that powered the system were hard-coded by software developers and managed in a manual process via decision tables in a Visual Basic application. This meant that if rules needed to be changed or added, a developer needed to spend a considerable amount of time making the modifications.
PROJECT OVERVIEW
The company decided to modernize its legacy system, prioritizing technologies that integrated with its existing Microsoft Dynamics CRM. The company’s solution had to empower its business users to write and manage rules, thereby freeing up technical staff to work on more strategic IT initiatives. The new solution also needed to automate the execution of business rules, eliminating time-consuming manual processes.
The healthcare company determined that the two elements of the application that would produce the greatest impact were billing and payables. By focusing on billing and payable functions first, the healthcare company could more accurately bill patients and providers and generate revenue faster. With this in mind, the healthcare company decided a decision platform would be the best solution to accomplish its goals.
SOLUTION
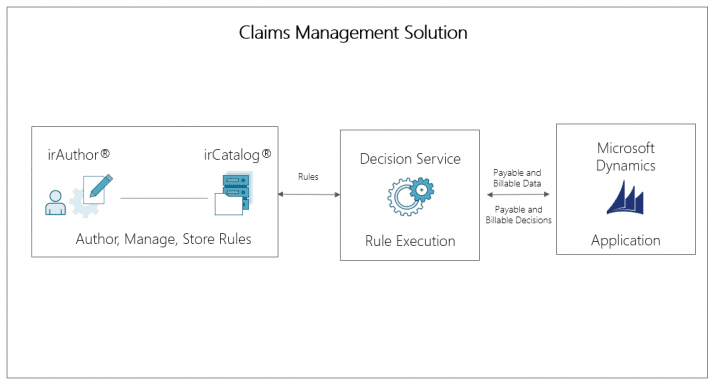
After considering a custom homemade web service, as well as solutions like Biztalk and Drools, the healthcare company selected InRule’s decision platform for its application.
The healthcare company chose InRule for its seamless integration with Microsoft Dynamics CRM and because its low-code platform alleviates the need for developers to write and maintain business rules in code. Additionally, decision makers recognized that InRule’s decision platform would provide the company the ability to build out more elements of the application, like determining which doctor to see or which drug to take, as the business continues to grow.
The healthcare company now leverages InRule to manage the business rules around contract terms for providers and patients. For example, InRule applies logic and rules toward all aspects of a patient visit and helps process the claim for that visit. The solution determines the amounts to be paid to the provider and the reimbursement to be paid back to the patient.
RESULTS
Since launching InRule, the healthcare company has realized tremendous cost and time savings. InRule has been integrated into Microsoft Dynamics CRM on-premises and is used to manage the financials for payables and billables. The solution has allowed the healthcare company to save time and money by deploying its IT staff to more strategic processes and allowing its business analysts to write and manage its decision logic. The company’s business logic is no longer split between decision tables and hard-coded into its application. Instead, the logic is centralized inside of InRule’s catalog (irCatalog®) in easy-to-reference business language.
A senior project leader said, “InRule just works, it’s easy to use and makes a real impact on our bottom dollar.”
Additionally, the healthcare company now has the ability to process more billing and payable claims than ever before. Thanks to InRule, the healthcare company has accelerated payment processes both for itself and vendors. The healthcare company is looking to expand its use of InRule for pharmacy, network, and referral management.
“InRule just works, it’s easy to use and makes a real impact on our bottom dollar.”
Senior Project Leader




